Journey in Caregiving
Helpful tips for family caregivers
July/August 2016
Seniors often lose the sensation of being thirsty. With the hot weather, there’s a good chance your relative may not be getting enough water. And speaking of “not enough,” we thought we’d give you a heads up about the things that are not covered by Medicare. We don’t want you caught up short. Last, we look at the concept of choice in caregiving. It’s common for families to operate on assumptions. Check out our tips for short-circuiting the resultant discord.
Is your relative dehydrated?
 If a person doesn’t drink much water, is it a big deal? In a word, yes!
If a person doesn’t drink much water, is it a big deal? In a word, yes!
Our bodies are 50%-60% water. The brain is more than 66% water. But we lose 2-3 quarts of fluid daily through normal body processes.
We need to replace that by drinking at least 6-8 glasses of water or nonsugar, noncaffeine, nonalcoholic beverages each day. That’s one glass every 2-3 hours. When the weather is hot, we need even more.
Between 20% and 40% of seniors regularly do not get enough water. The result is dehydration, which can have a variety of effects. The most common problems include:
- constipation
- confusion
- dizziness and falls
- bladder infections
- pressure ulcers, also known as bed sores
How do you know if your loved one is dehydrated?
Thirst may be a sign, but it’s unreliable. Many older adults lose the sensation of thirst. A dry or sticky mouth or headaches can signal dehydration. Muscle weakness, sleepiness, and tiredness are also signs. Dark urine is a sure sign.
The solution for dehydration is simple: Have your relative drink more water! But remember, he or she may have no thirst. Here are friendly ways to support more fluid intake:
- Start slow. If your loved one drinks three glasses a day, shoot for four until that becomes a habit. Then you can increase by another glass.
- Understand the barriers. Often people are afraid to drink more because they’ll have to urinate more, and at inconvenient times.
- Keep a pitcher of water out and handy all day.
- If you are visiting, pour a glass of water regularly. Don’t ask, just pour one for yourself and hand one to your loved one.
- Make water drinks appealing. Add a bit of lemon, or cucumber, or mint.
- Try a sugar-free beverage if more flavor is needed.
Whose idea was this, anyway?
 If the role of “chief caregiver” for Mom or Dad was not one you chose, you are not alone. According to a study by the American Association of Retired Persons and the National Alliance for Caregiving, 49% of family caregivers feel they really did not have a choice in the matter. There are several factors:
If the role of “chief caregiver” for Mom or Dad was not one you chose, you are not alone. According to a study by the American Association of Retired Persons and the National Alliance for Caregiving, 49% of family caregivers feel they really did not have a choice in the matter. There are several factors:
The tyranny of the first-born. Across many cultures, it is assumed that the first-born will be in charge of the parents’ care, especially a daughter. Everyone defers to the eldest for decisions.
A twist of geography. Sometimes, by default, family members rely most heavily on the adult child who lives nearby.
“Mom likes you best.” Although we might wish it weren’t so, the truth is, parents have favorites. The child with the “closest” relationship is often expected to step in, even when a different sibling is more available or has better caregiving skills.
No matter which is the case, being the caregiver is often an isolating and overwhelming role. Particularly so when there is criticism and pushback by siblings.
Take these steps to reduce family conflict and your own feelings of resentment:
- Bring assumptions into the open. Have a family meeting, with your parents there too. Talk about care needs and wishes. Discuss the options as a group.
- Align decision making with the day-to-day caregivers. Nothing builds resentment more than having one child provide the hands-on care while another calls the shots.
- Divide roles based on ability. It may be that the physically closest child is the best suited to drive mom on errands. But spread around the other tasks, such as managing the finances or researching medical issues.
- Keep everyone informed. Conflict is less likely to occur if all siblings are kept in the loop. Avoid last-minute surprises with a weekly email talking about current issues and concerns.
What Medicare does NOT cover
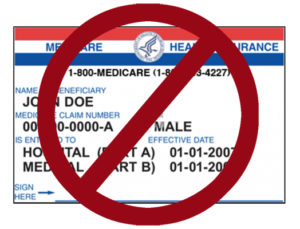 Medicare is health insurance for those over age 65. A surprising number of things that might seem obvious as health needs of elders are not included as benefits. This can get costly!
Medicare is health insurance for those over age 65. A surprising number of things that might seem obvious as health needs of elders are not included as benefits. This can get costly!
For example, in the normal process of aging, many older adults need glasses, hearing aids, and sometimes dentures. Foot problems are also common. But Medicare does not cover
- vision problems. Routine eye exams and corrective glasses are not covered. Patients with high-risk diseases, however, such as diabetes and glaucoma, can be screened yearly. And cataract surgery is covered.
- hearing problems. Testing to confirm hearing loss is covered. But hearing aids must be paid for out of pocket.
- dental care. Anything routine, such as teeth cleaning, cavity repair, or dentures, is not covered. Dental surgery or care required because of a disease, such as cancer, is covered.
- foot care. Injuries and diseases, such as bunions and bone spurs, are covered. But treatment for common gripes, such as calluses and tough toenails, must be paid for privately.
Similarly, age-related changes in health often lead to a need for help with basics, such as bathing, dressing, and cooking. And many seniors can’t live safely by themselves. But Medicare does not pay for assistance at home. And it does not cover long-term “custodial” care in a facility.
Isn’t retirement a time to travel? If you get sick outside the United States, Medicare will not pay for medical care or hospitalization. (There are exceptions if you are just over the border or on a cruise ship that has recently left port.)
Complimentary medicine, such as acupuncture and chiropractic care, is not covered. Nor is elective cosmetic surgery.
If your relative needs more than what basic Medicare provides, check into the options. “Medicare Advantage” plans may cover additional services.
Return to top
